1. TREATMENT PLAN & GOAL LINKAGE ENHANCEMENT
Overview
In this release, we’ve enhanced Practice EHR by introducing a new feature that allows treatment plans to be linked directly to patient goals.
This update allows treatment plans to be directly linked to patient goals, enhancing workflow automation and care coordination. A new "Goals Bucket" has been added to the treatment plan, providing easy access to unresolved goals and associated treatment plans.
Additionally, the sentence view for Recommendation has been renamed to Treatment Plan to better reflect the details documented in the progress note. The previously generated sentence view descriptions for scheduled procedures and medications, formerly known as protocols, have been removed and are now consolidated under the Treatment Plan to provide a more streamlined approach to documentation.
Key Enhancements
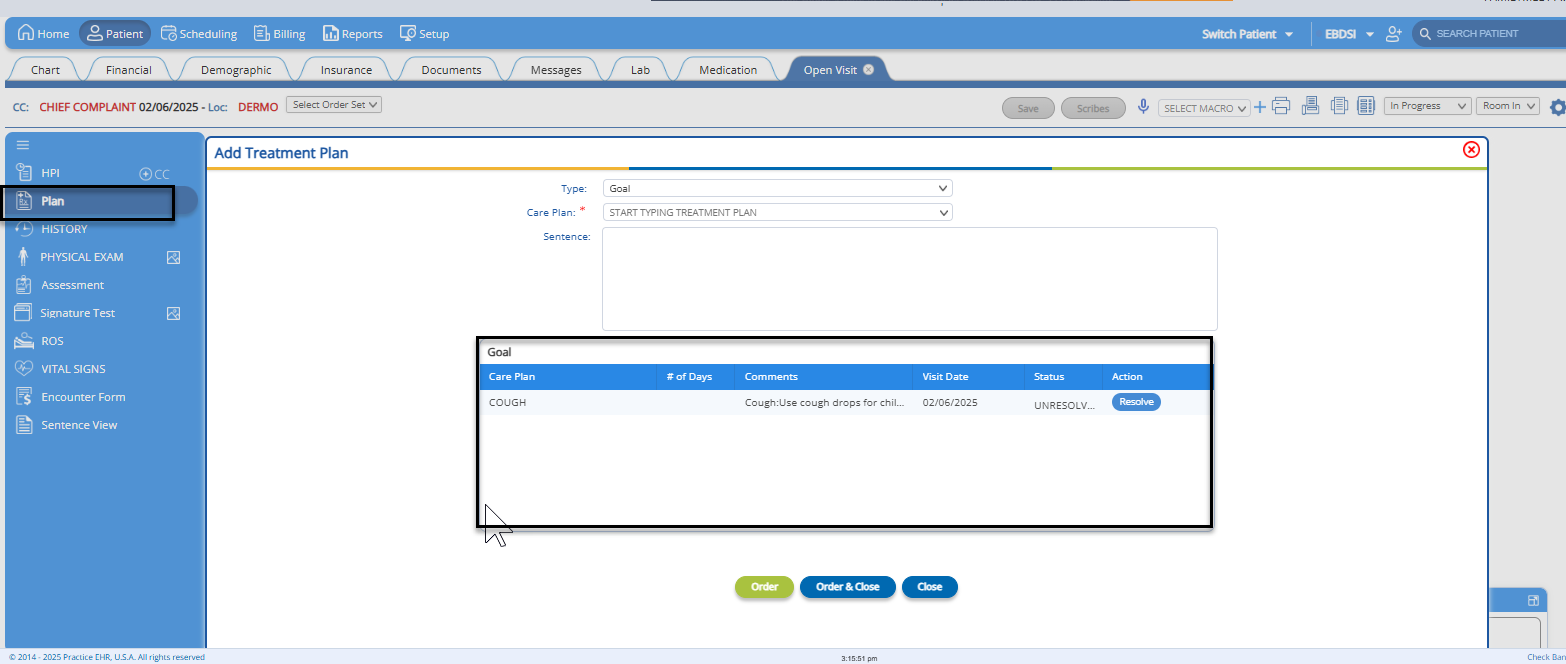
- Goal Bucket Addition: A new section under Clinical Visit > Plan > Add Treatment Plan displays unresolved goals. Users can add, track, and resolve goals.
- Treatment Plan Linkage: Users can link treatment plans to goals, ensuring alignment with patient care objectives.
Benefits
- Enhanced Goal-Oriented Care: Aligns treatment plans with patient goals.
- Improved Workflow Efficiency: Quick access to treatment plans and goals reduces clicks and improves productivity.
- Streamlined Patient Follow-Up: Automated notifications ensure timely care coordination.
- Reduced Administrative Burden: Automation decreases manual tracking and enhances staff efficiency.
- Increased Patient Engagement: Follow-ups improve adherence to treatment plans.
How it Works:
- Adding Treatment Goals
- Under the Clinical Visit > Plan > Add Treatment Plan section, a new Goal bucket has been added. Once a goal is ordered, it will appear in the Goal bucket.
- Additionally, all previously unresolved goals will be listed in this bucket. Users can add new goals to the bucket or resolve any unresolved goals by clicking the 'Resolve' button once they have been addressed.
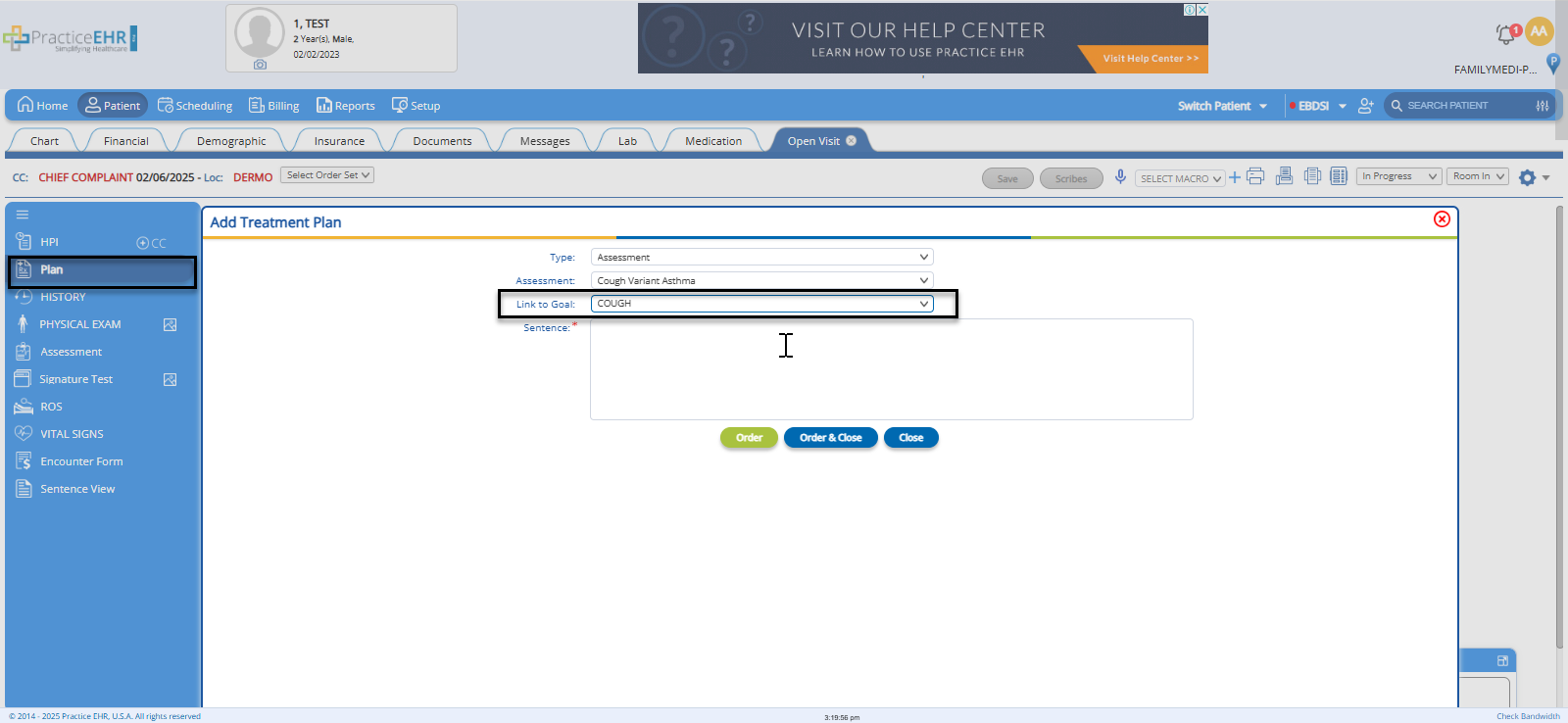
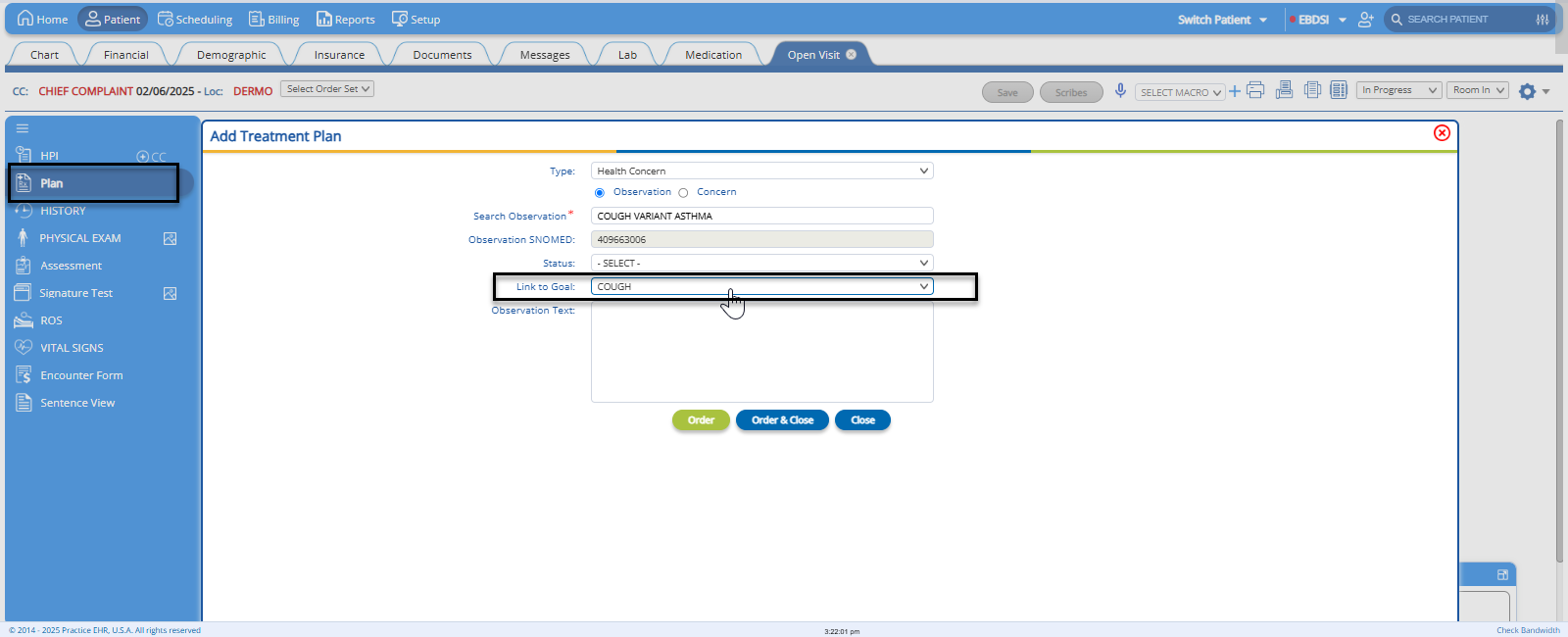
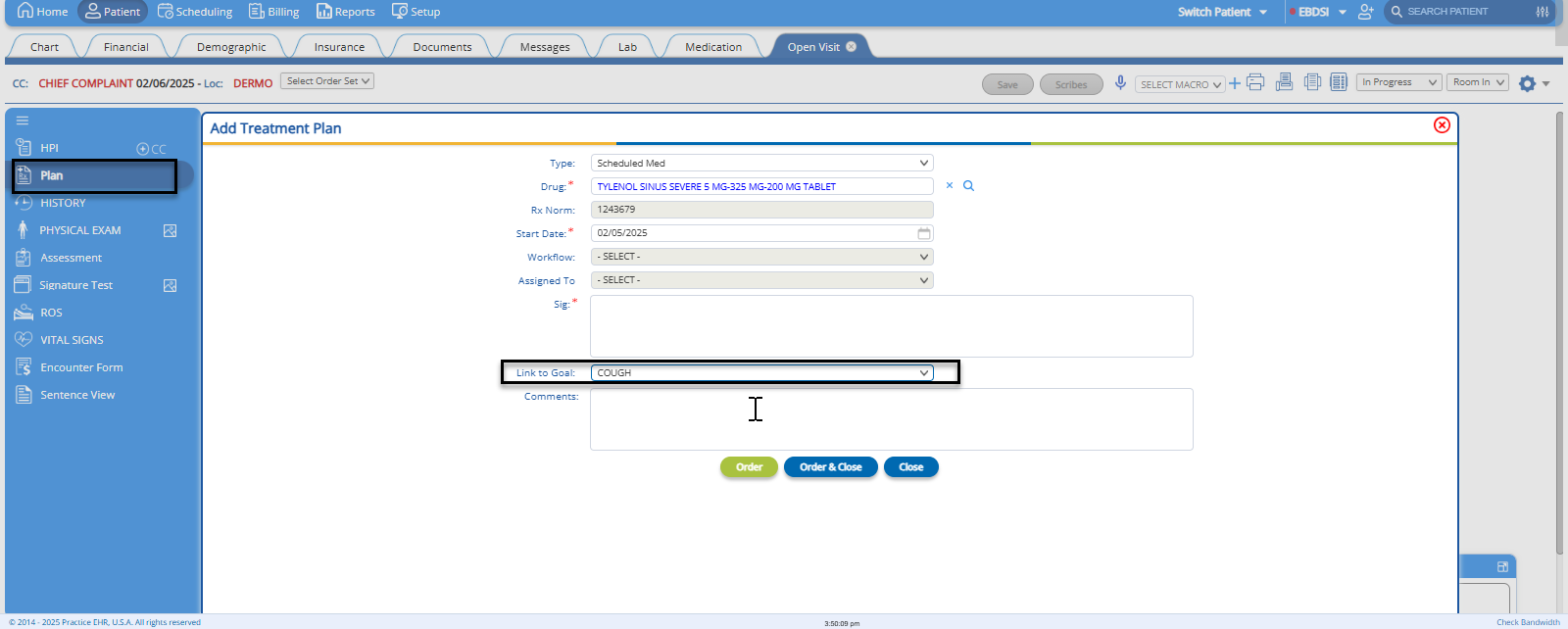
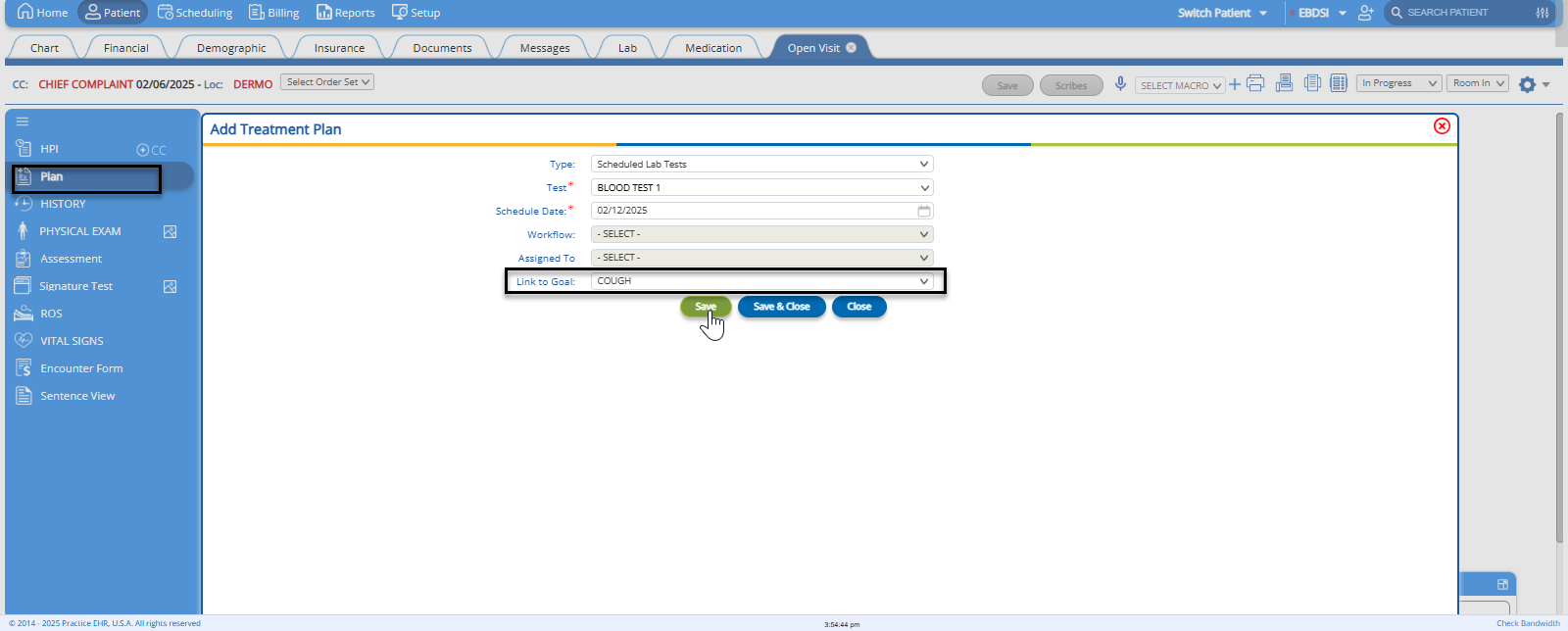
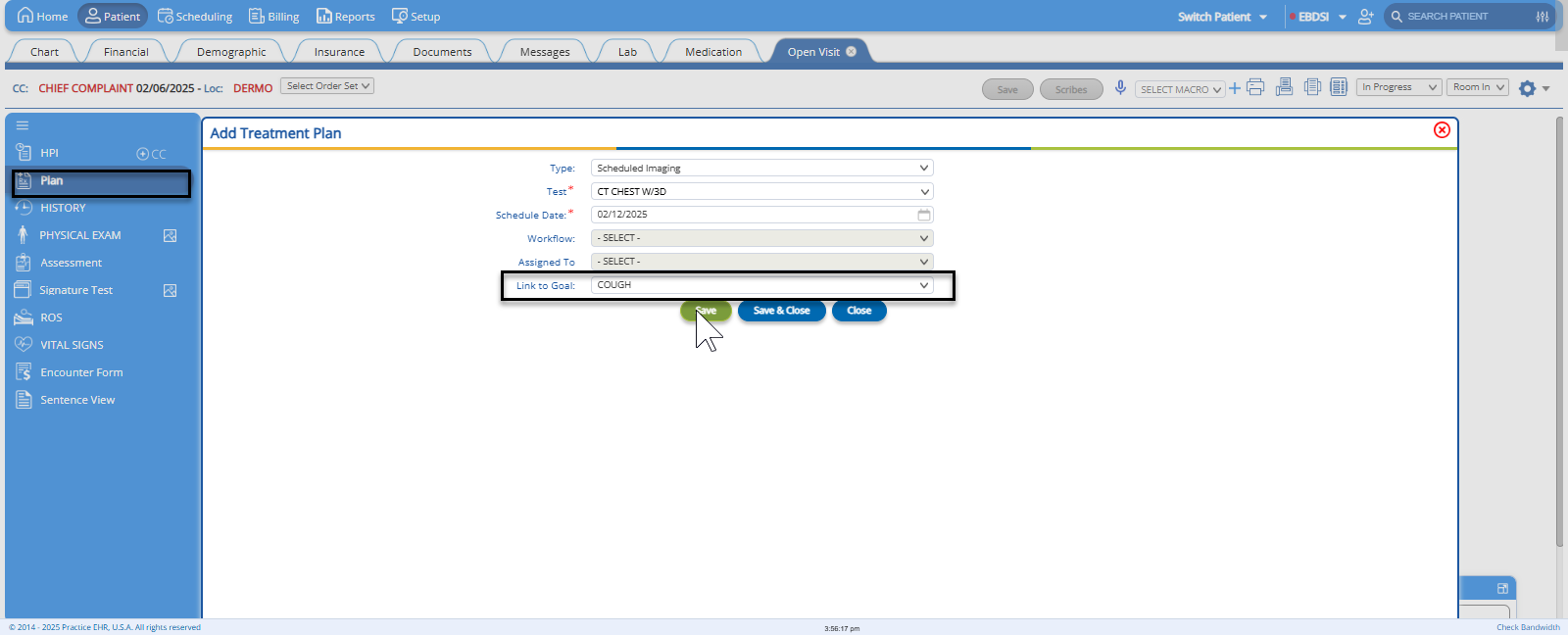
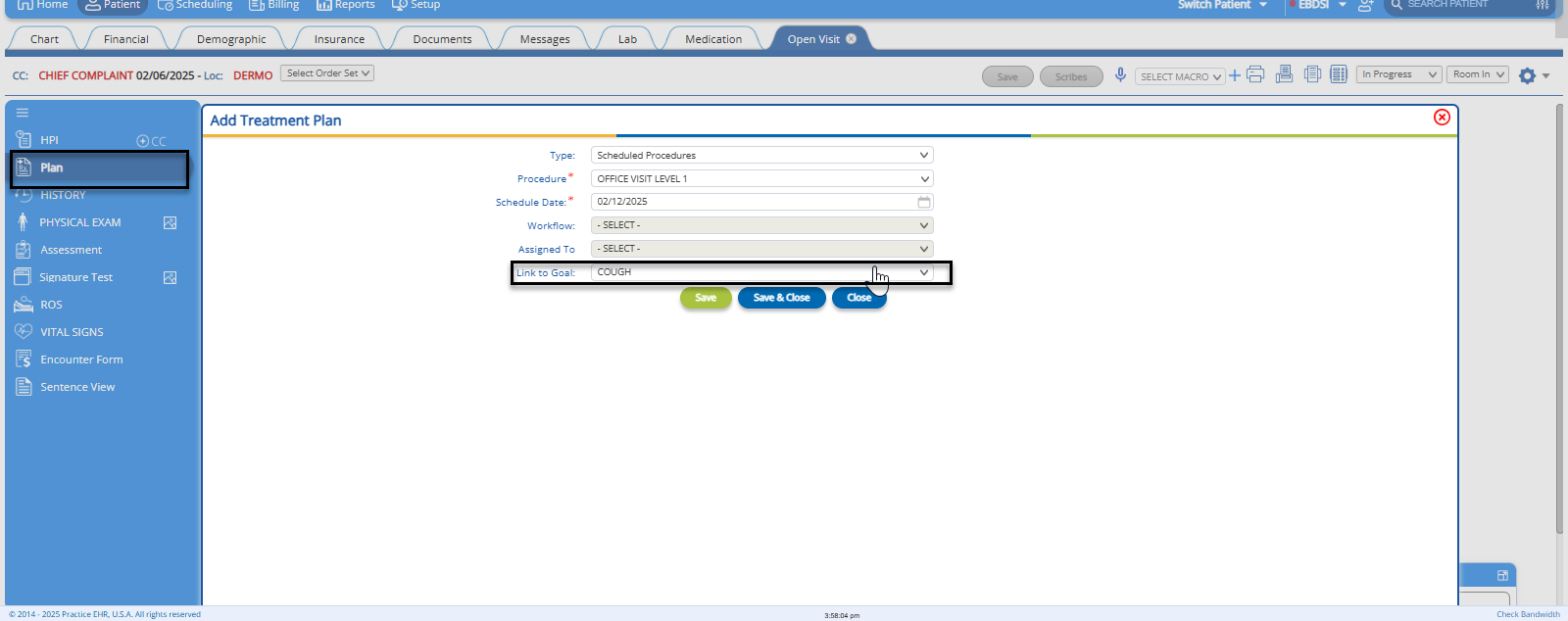
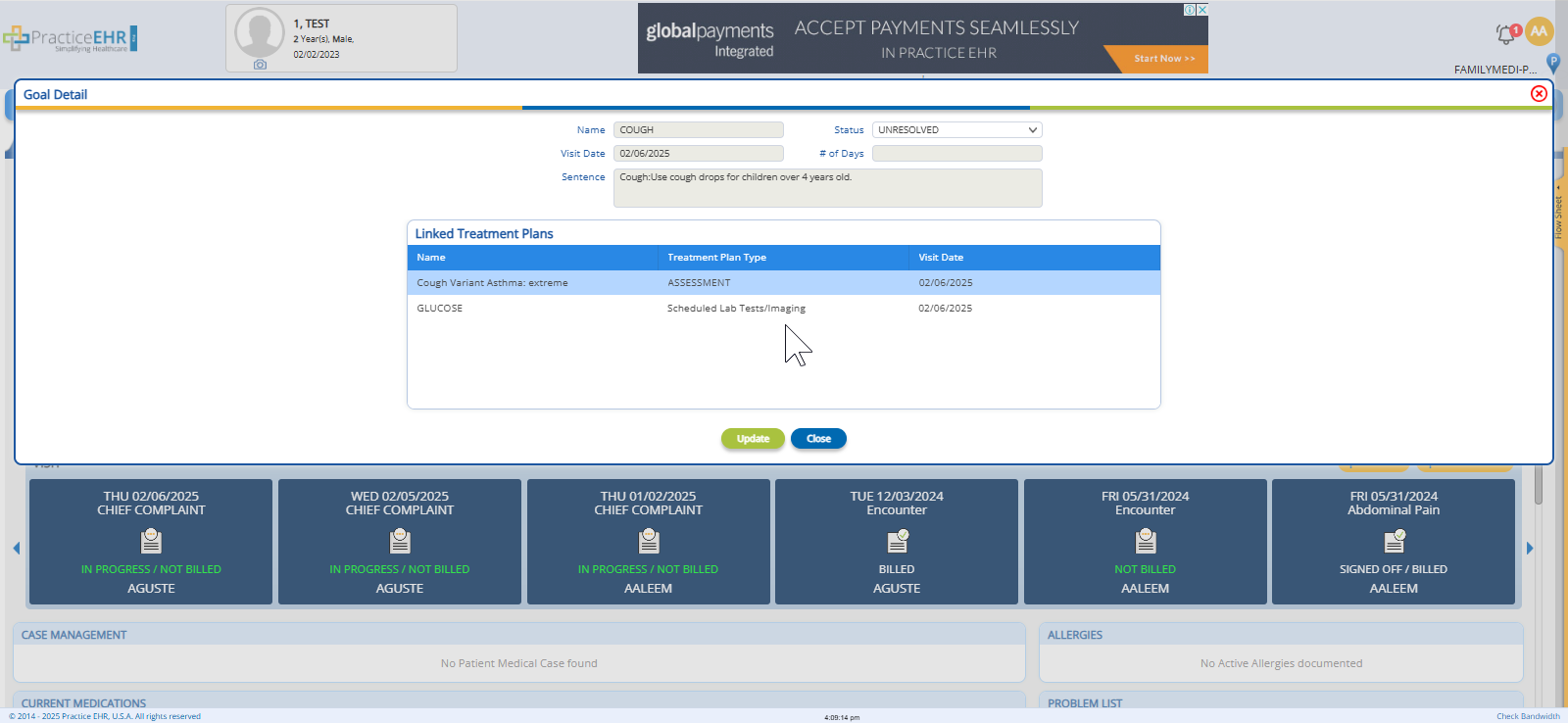
- Linking Treatment Plans to Goals
- Users can now link treatment plans directly to specific patient goals, ensuring that the treatment plans align with the intended outcomes for the patient’s care.
- Under the Clinical Visit section, users can now add treatment plans to goals. The linked treatment plans include:
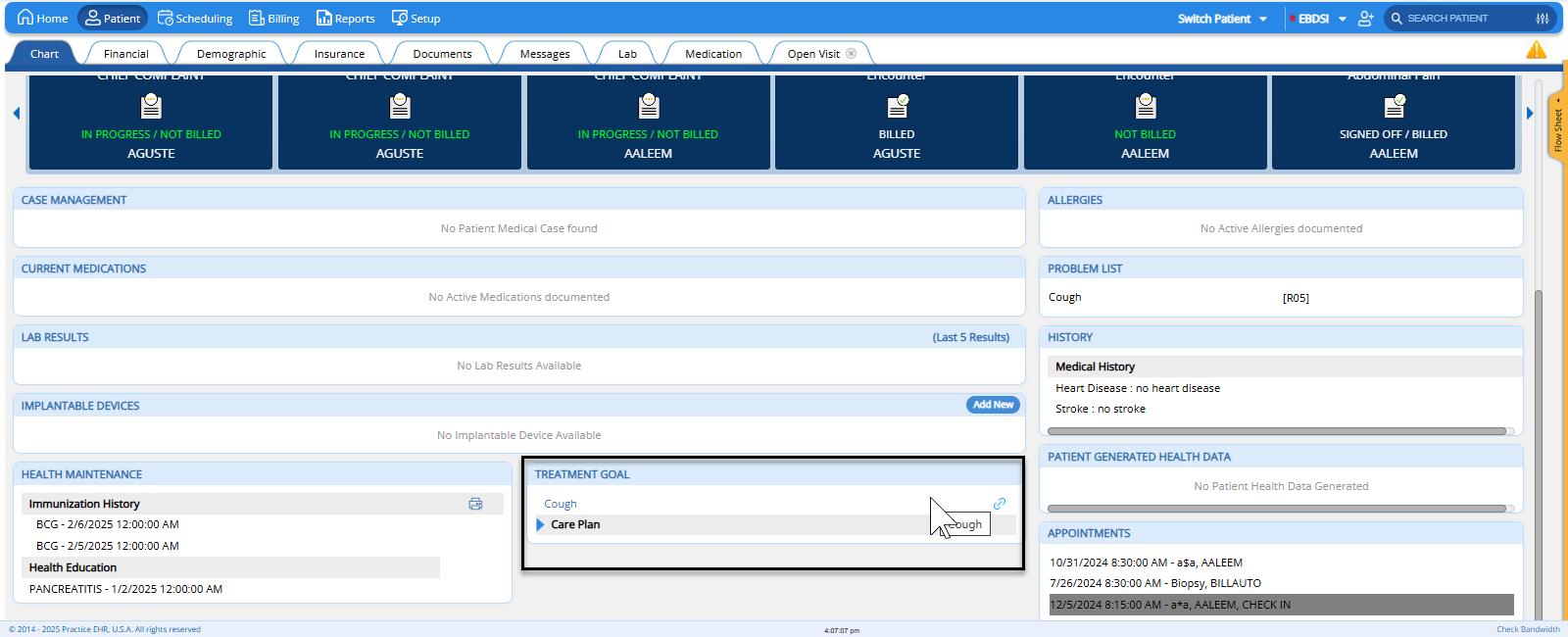
- Treatment Goals Bucket on Patient Chart
- A new section, Treatment Goals, has been added to the patient chart, displaying all the patient’s goals
Users can click on any goal to view all treatment plans that are associated with that goal, enhancing visibility and ease of navigation.
Benefits of This Enhancement:
- Enhanced Goal-Oriented Care:
- By linking treatment plans to patient goals, healthcare providers can ensure that all aspects of care are aligned with the patient’s specific objectives. This creates a more targeted approach to treatment, improving care outcomes.
- Improved Workflow Efficiency:
- The addition of the Treatment Goals Bucket and the ability to quickly view linked treatment plans improves the workflow, allowing providers to access essential information with fewer clicks. This reduces time spent searching for patient data, increasing productivity.
- Improved Care Coordination Across Teams:
- The treatment follow-ups and the clear visibility of linked goals and treatment plans ensures that multiple care providers or teams can stay informed and aligned on the patient’s care plan. This can lead to fewer gaps in care and a more integrated treatment approach.
2. MENU REARRANGEMENT IN SETUP TAB
Overview
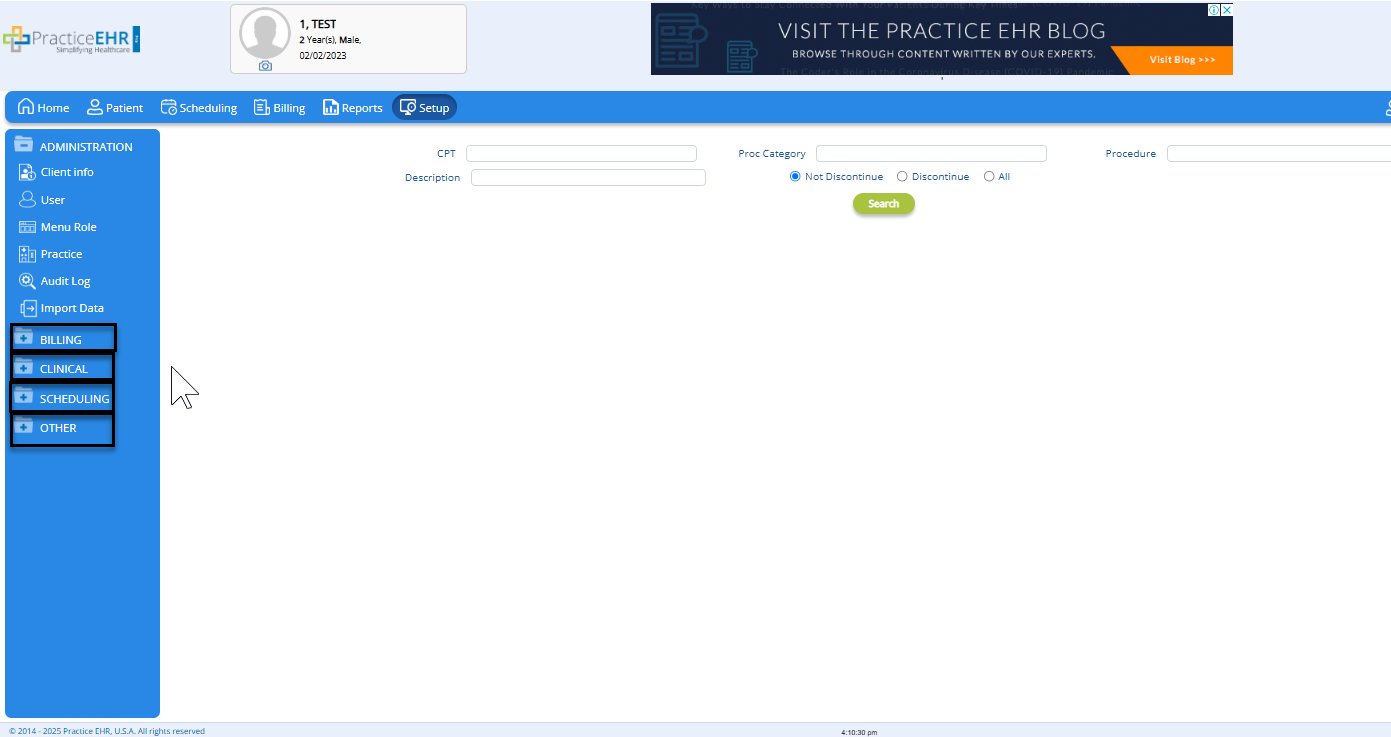
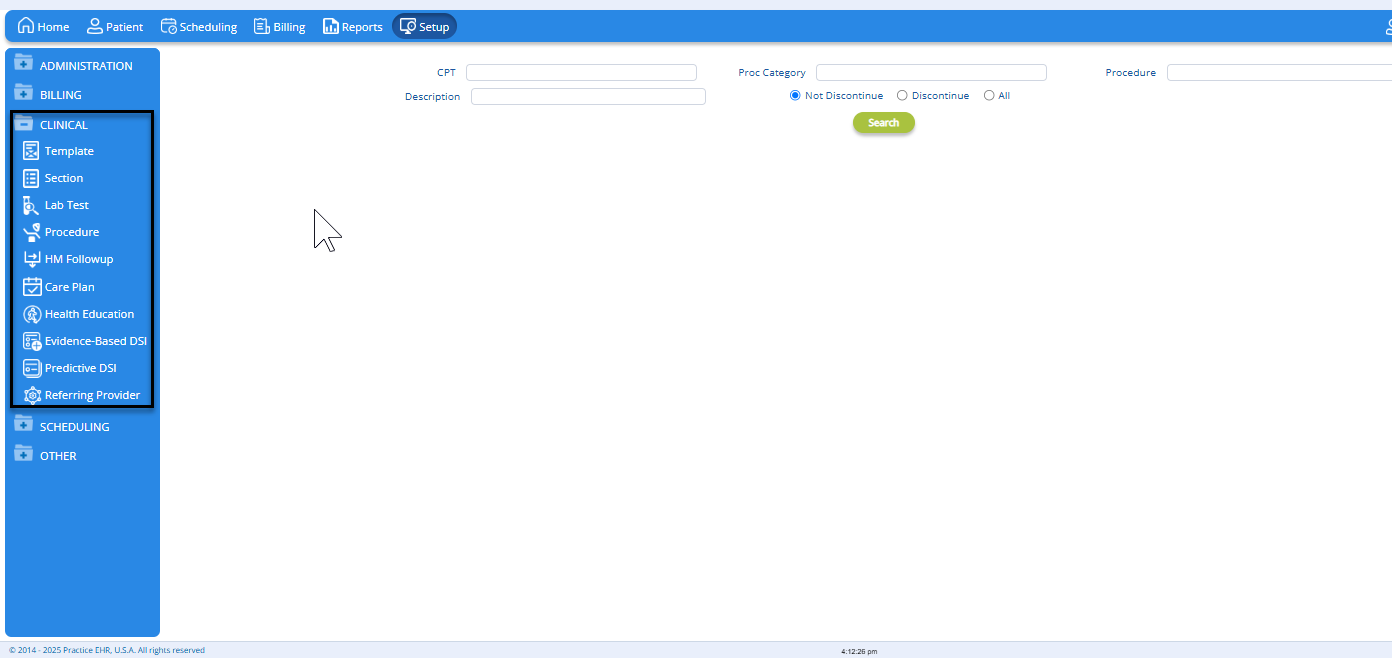
In this release, we’ve reorganized the menus under the Setup tab to enhance navigation and improve user experience. The Setup tab has been reorganized for improved navigation and efficiency. Menus are now grouped under subcategories to provide easier access to settings.
We’ve also made changes to the Clinical Designer menu to streamline the organization and improve navigation. All subcategories that were previously housed under Clinical Designer — including Visit Templates, Sections, and Clinical Profiles — have now been moved under the Clinical Profiles heading as separate, easily accessible items. This restructuring enhances user experience by simplifying access to these critical settings.
Key Changes:
- Reorganized Menu Structure
- The Setup tab has been reorganized to better group related settings together. This provides a more intuitive structure for users to find the configurations they need.
- New Subcategories Under Profile Heading
- The following subcategories have been added under the Profile heading:
- Billing
- Clinical
- Scheduling
- Others
- These subcategories will now house relevant settings and configuration options for each specific area, making them easier to locate.
- Improved Navigation and Usability
- The changes aim to provide a more streamlined experience by minimizing the number of clicks required to access frequently used settings.
- Users can now quickly jump to the relevant section within the Profile menu, reducing clutter and simplifying navigation.
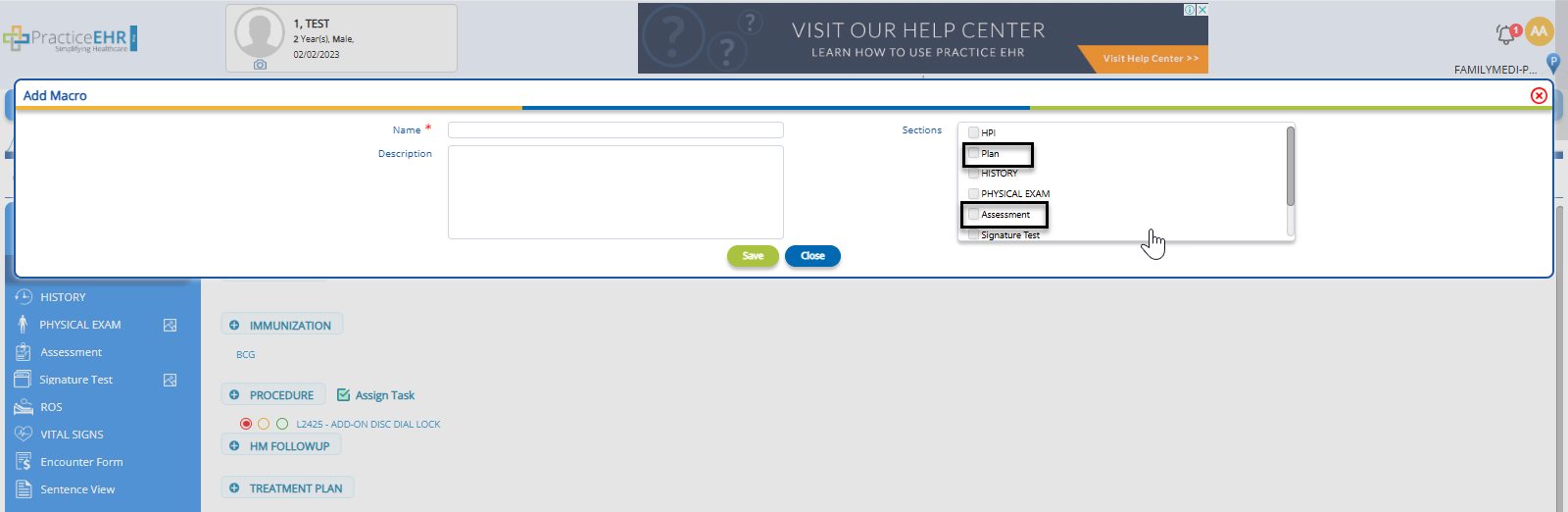
3. MACRO ENHANCEMENT FOR PLAN & ASSESSMENT SECTIONS
Overview
In this release, we’ve expanded the macro functionality introduced in the previous release by adding the ability to create macros for the Plan and Assessment sections. This enhancement allows users to create customizable templates for these critical areas, further improving workflow efficiency and standardizing clinical documentation. Now, providers can quickly insert pre-defined content into the Plan and Assessment sections of patient visits, reducing the time spent on routine documentation.
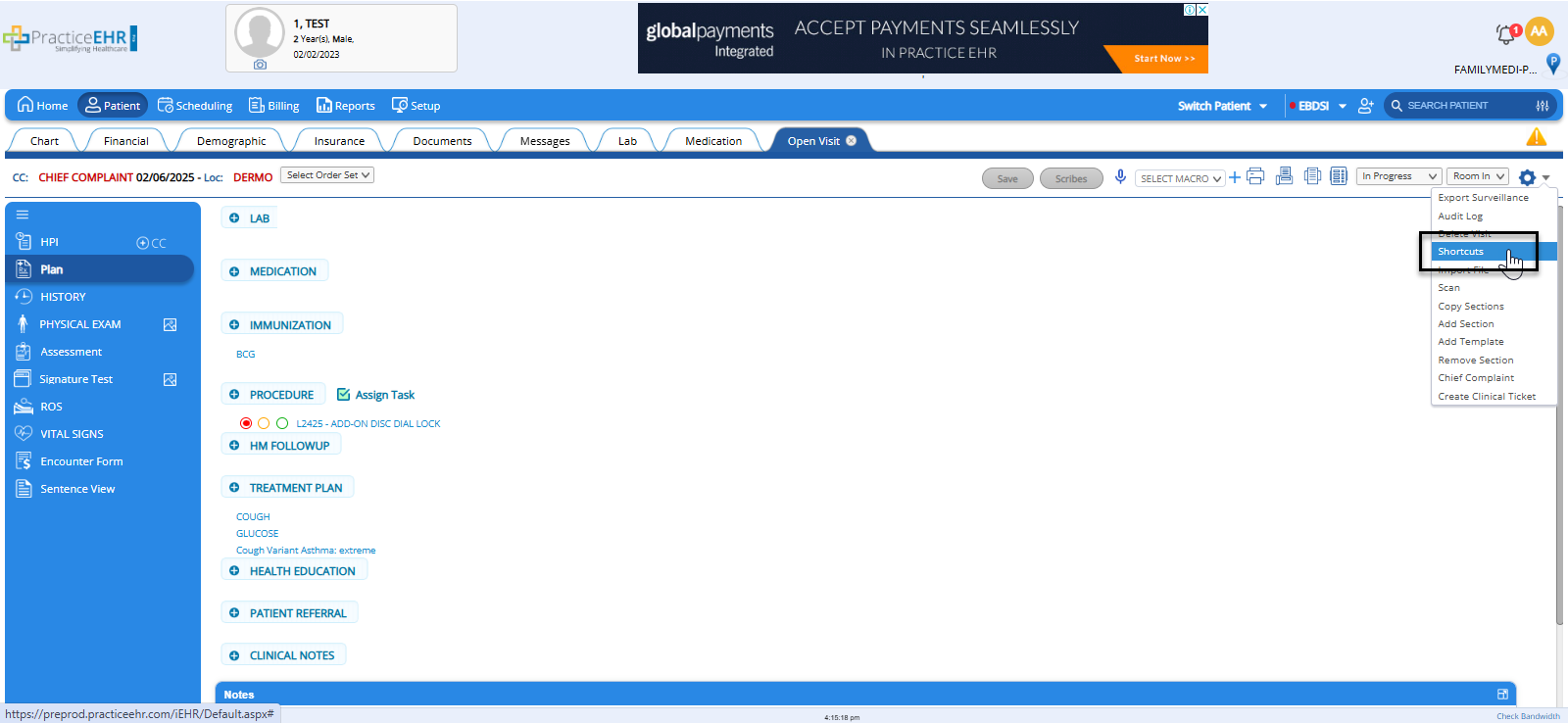
We have also made a minor but important change to the user interface to enhance clarity and streamline user navigation. The Macro option under the Clinical Visit gear icon has been renamed to Shortcuts. This change better reflects the functionality of the feature, providing users with quicker access to frequently used actions, phrases, and templates, which are now categorized as "Shortcuts."
There is no disruption to the way the feature works. The renaming is purely cosmetic, meaning users can continue working with their existing shortcuts seamlessly.
4. AI CLAIM EDITING
Overview
As part of a beta launch, we have introduced a new AI Claim Editing feature to further enhance the claims management process. When a provider marks a claim as Ready to Bill, the claim will land in the Claim Editing Bucket, where various plan-level editing rules are applied to ensure there are no issues. In addition to this, our new AI functionality evaluates the rejection probability of the claim before it is moved to the Submission Bucket. This added layer helps reduce claim rejection rates by providing early warnings and suggestions that assist users in making more informed decisions before submitting claims.
This feature is enabled by request only. Clients are requested to reach out to support for activation.
How It Works:
- Marking Claims as Ready to Bill
- When a healthcare provider or billing staff marks a claim as Ready to Bill, the claim enters the Claim Editing Bucket. This is where plan-level editing rules are applied to check for common errors or inconsistencies. Typically, this includes verifying coding, payer requirements, and general claim structure.
- AI Rejection Probability Evaluation
- After the claim passes the standard plan-level editing checks, an AI algorithm is triggered. The AI evaluates the claim's details using historical data and machine learning models to predict the probability of claim rejection. The AI analyzes:
- Claim content such as coding, modifiers, and diagnoses
- Payer-specific requirements based on past claim rejection patterns
- Claim history, including past rejections or common issues for similar claims
- Regulatory compliance, ensuring all necessary fields are filled and accurate.
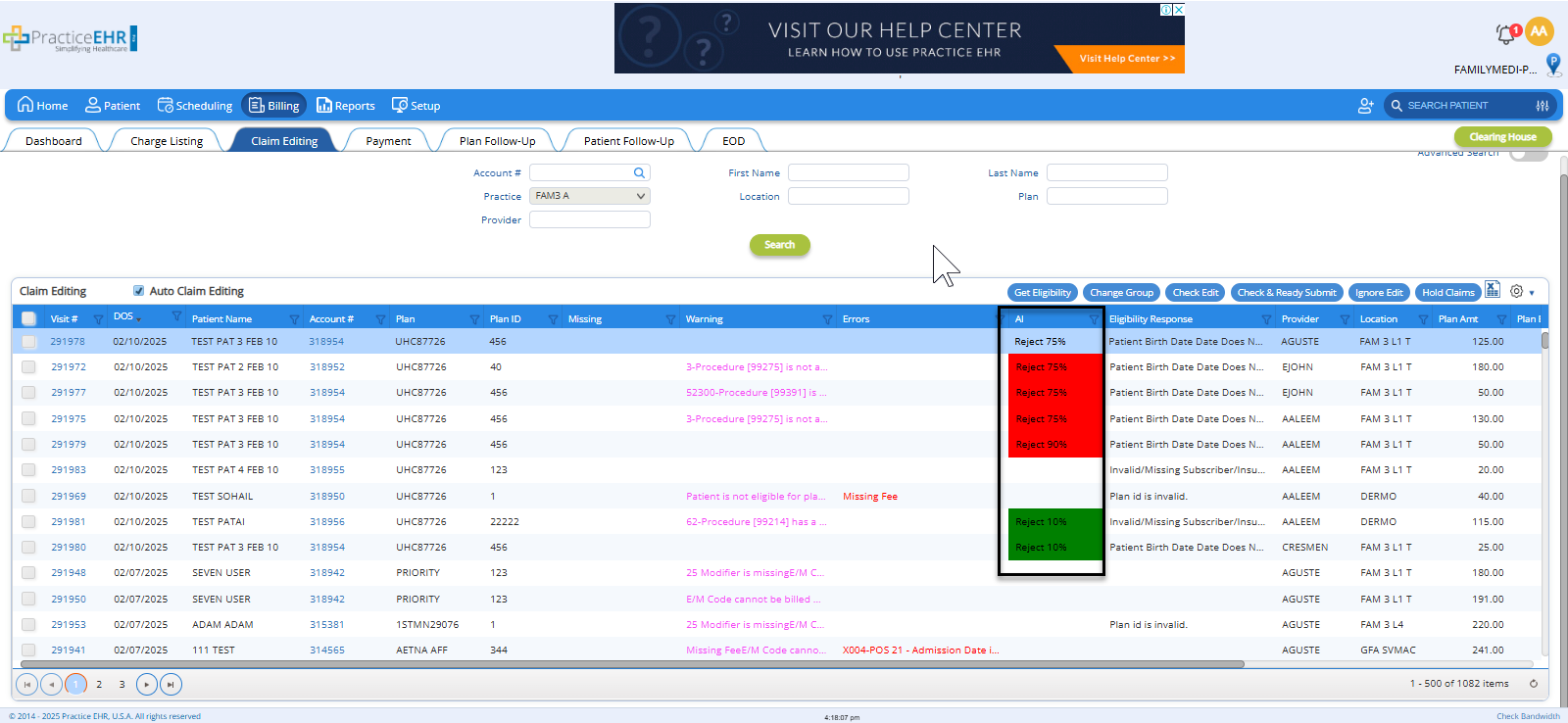
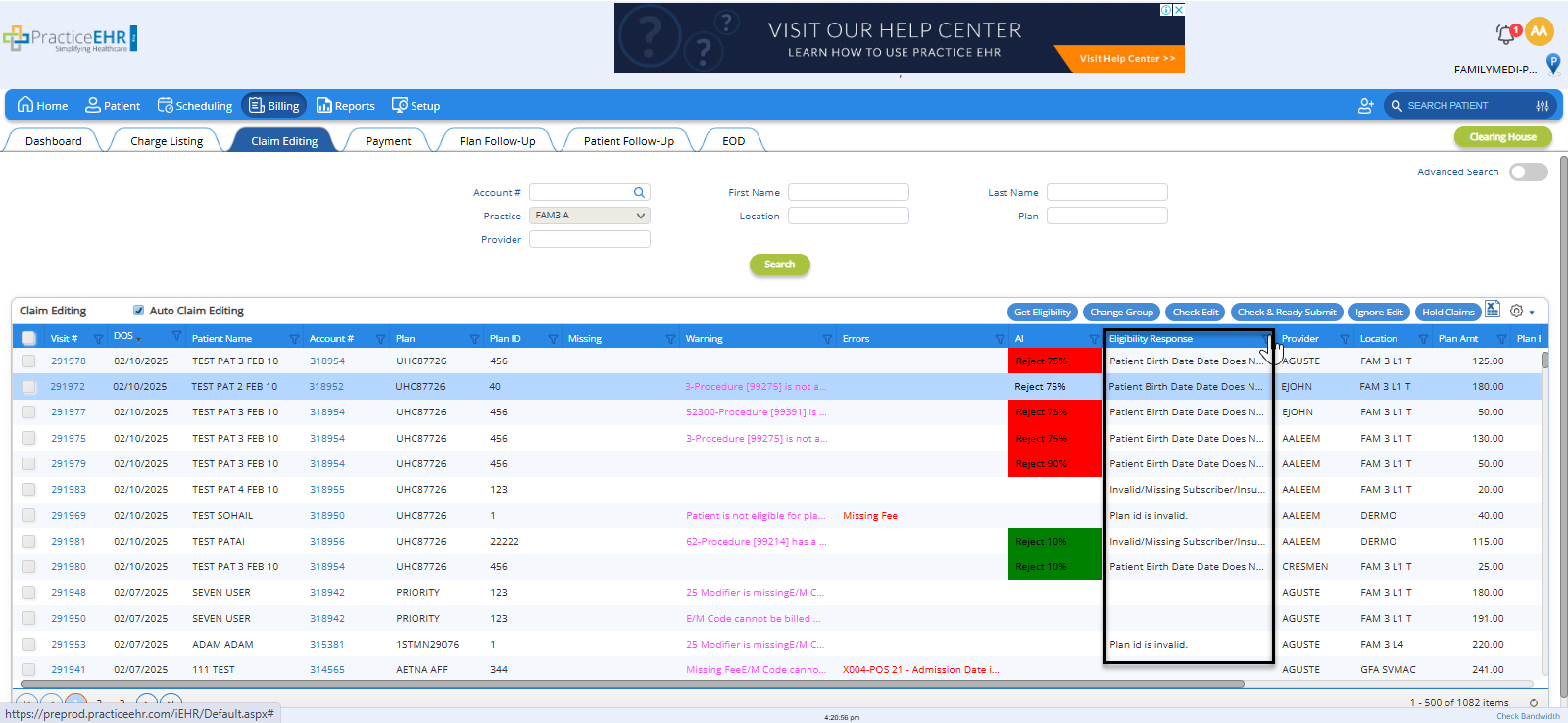
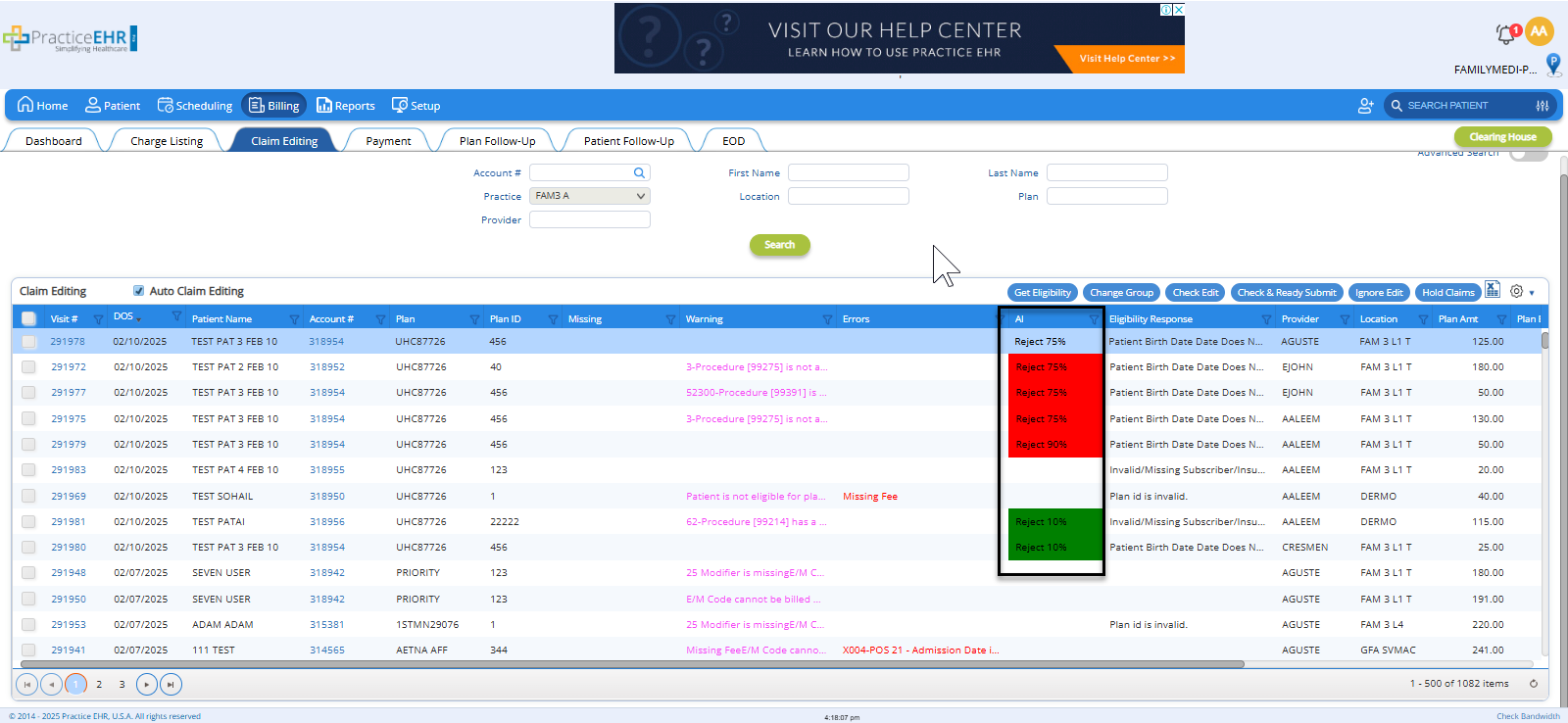
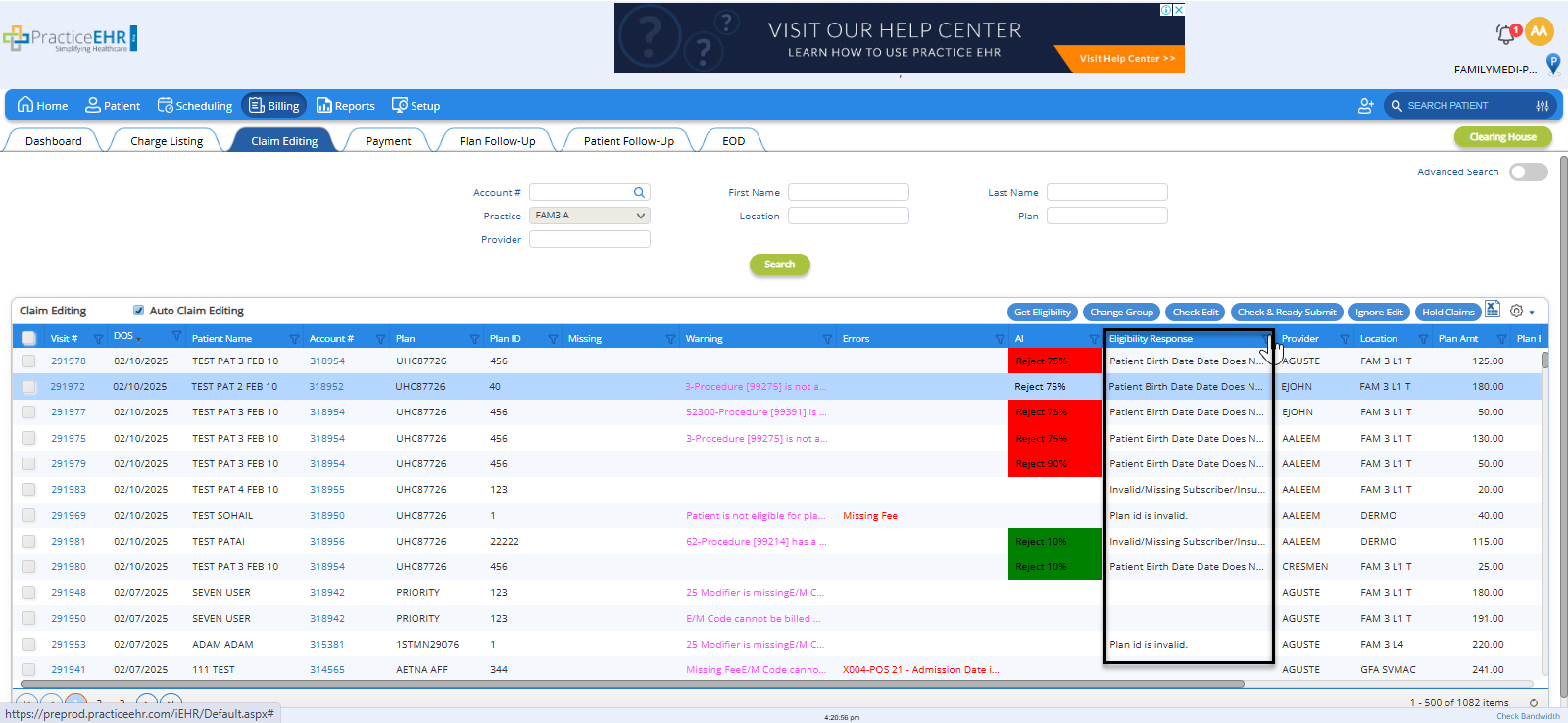
- A new column titled AI has been added to the Claim Editing Bucket, displaying the claim rejection probability. If a claim is likely to be accepted upon submission, it will be marked as ‘Accept.’ Otherwise, the column will show the rejection probability for the claim, as shown in the screenshot below.
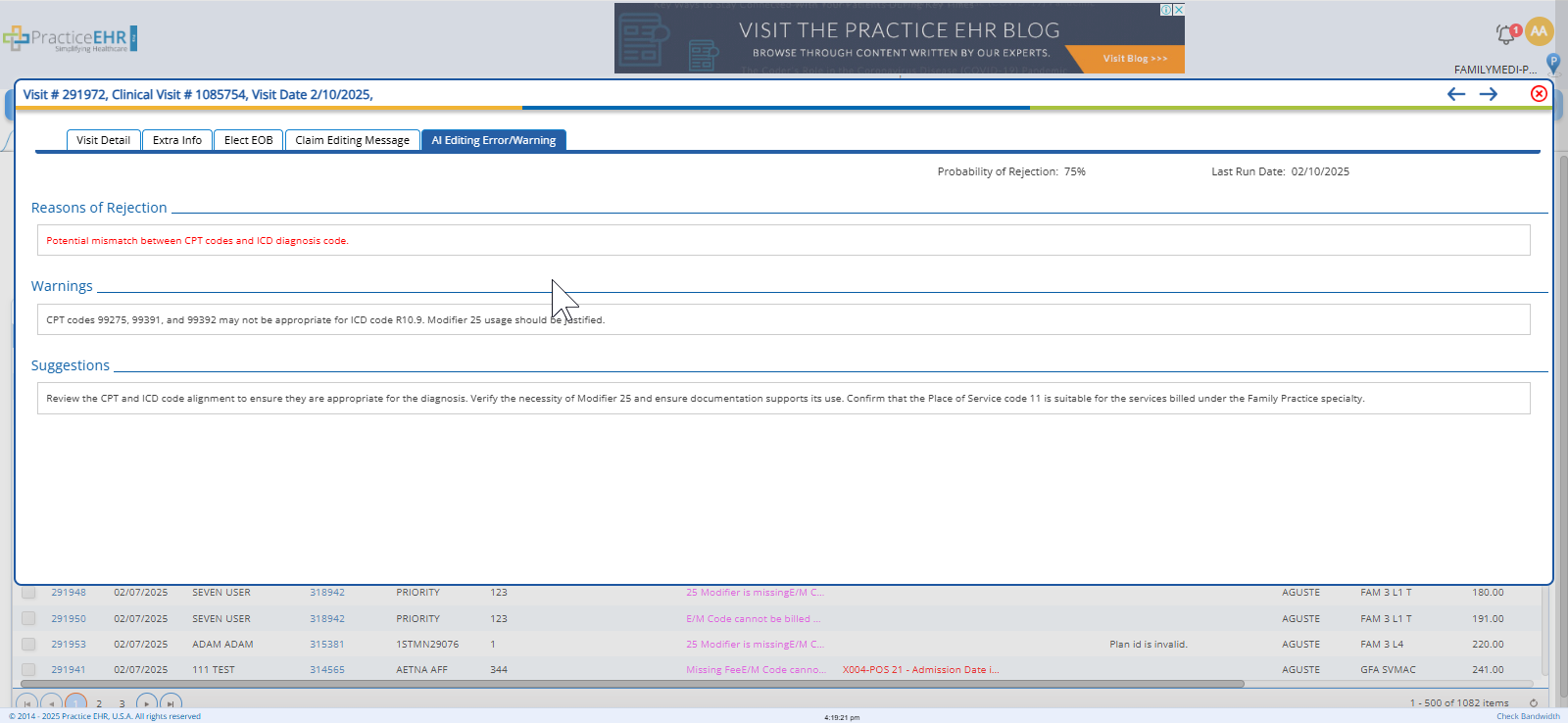
- If AI predicts the reject probability for the claim, the detail can be seen under the Visit Detail > AI Editing Error/Warning.
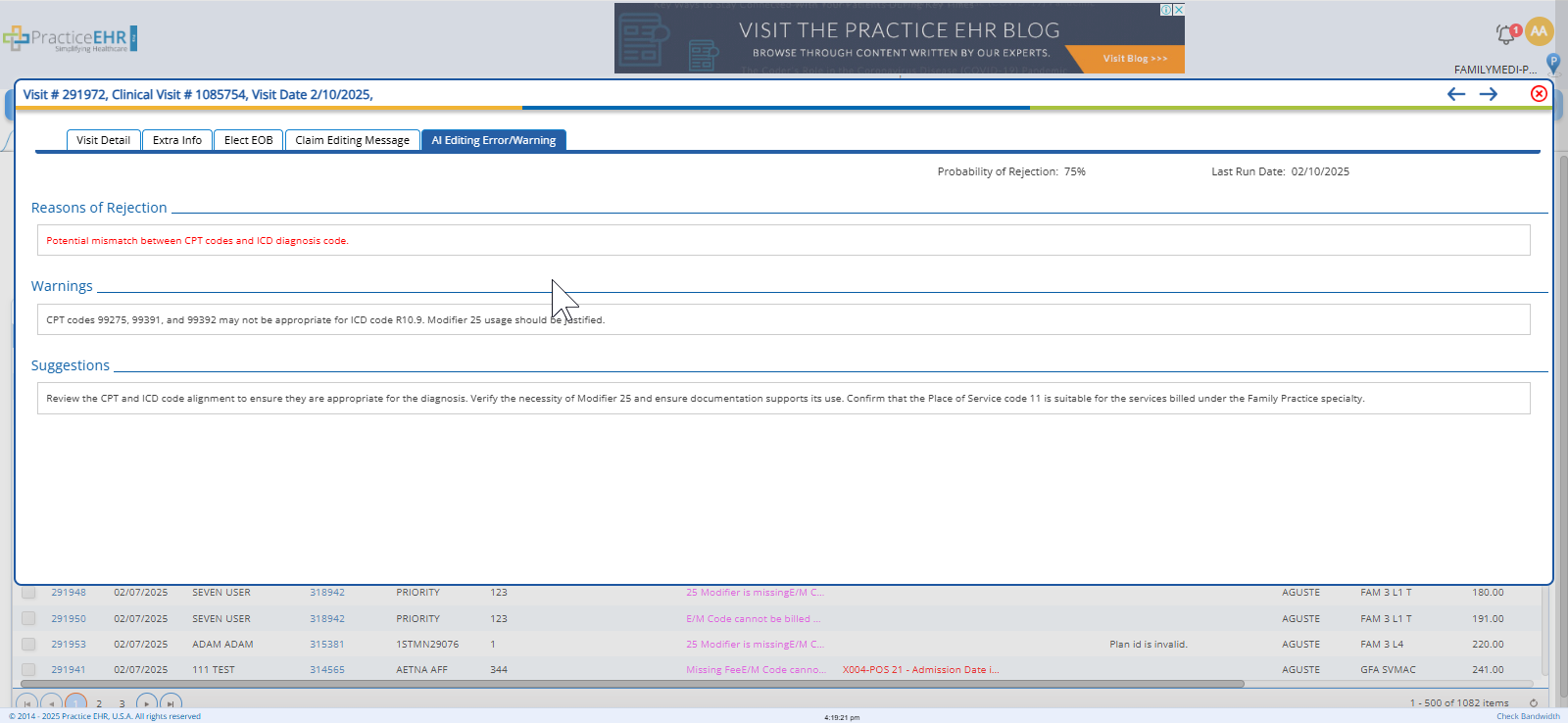
- Warning, Suggestions, and Rejection Probability
- The system presents the AI’s feedback in a clear and actionable way:
- Warnings: Indicating that there are high-probability issues that could lead to a rejection.
- Suggestions: Offering alternatives or changes to improve the claim’s chances of approval.
- Rejection Probability Score: Displaying a percentage that shows how likely the claim is to be rejected based on the AI’s evaluation.
- Example: The AI may flag a claim for a missing modifier with a warning such as “Possible rejection due to missing modifier for procedure code,” accompanied by a 70% rejection probability.
- User Flexibility
- Ignoring Warnings: Users can choose to ignore the warnings, suggestions, and rejection probability provided by the AI. The system allows claims to be moved to the Submission Bucket even if AI has flagged potential issues. This gives users flexibility and control over the final decision, especially in cases where they may have additional context or feel confident the issue is not relevant.
Benefits of This Enhancement:
- Reduction in Claim Rejection Rates:
The AI-powered validation helps identify potential issues before claims are submitted, reducing the chances of claims being rejected or denied due to common errors or payer-specific rules.
- Improved Decision-Making:
By presenting warnings, suggestions, and rejection probability assessments, this feature enhances decision-making during the claim submission process. Users can review potential issues and adjust as necessary to improve the likelihood of approval.
- Faster, More Efficient Claims Processing:
The automated AI validation provides an additional layer of review without requiring manual intervention, speeding up the claims process. Providers and billing teams no longer need to manually check for rejection risks, saving time while improving accuracy.
- User Flexibility:
While the AI highlights potential issues, users still have the option to override or ignore these warnings and proceed with claim submission. This flexibility allows for human judgment to play a role in complex or nuanced claim situations.
- Enhanced Claims Accuracy:
With AI flagging potential issues early, claims are more likely to be complete and compliant with payer requirements. This improves the accuracy of submitted claims and increases the chances of timely reimbursement.
- Better Insights into Claim Issues:
AI-generated warnings and suggestions provide detailed feedback on the claim, offering insights that can help the user better understand why a claim might be rejected. This helps to improve the accuracy of future claim submissions and enhances overall billing workflows.
5. ELIGIBILITY IN CLAIM EDITING MODULE ENHANCEMENT
Overview
In this release, we’ve added the Eligibility feature to the Claim Editing Module to provide billers with critical information that can help them make more informed decisions before submitting claims. This feature enables users to check a patient’s eligibility status directly within the claim editing process, streamlining claim management and improving accuracy. By integrating eligibility information, we aim to reduce errors and ensure that claims are more likely to be accepted upon submission.
How it Works:
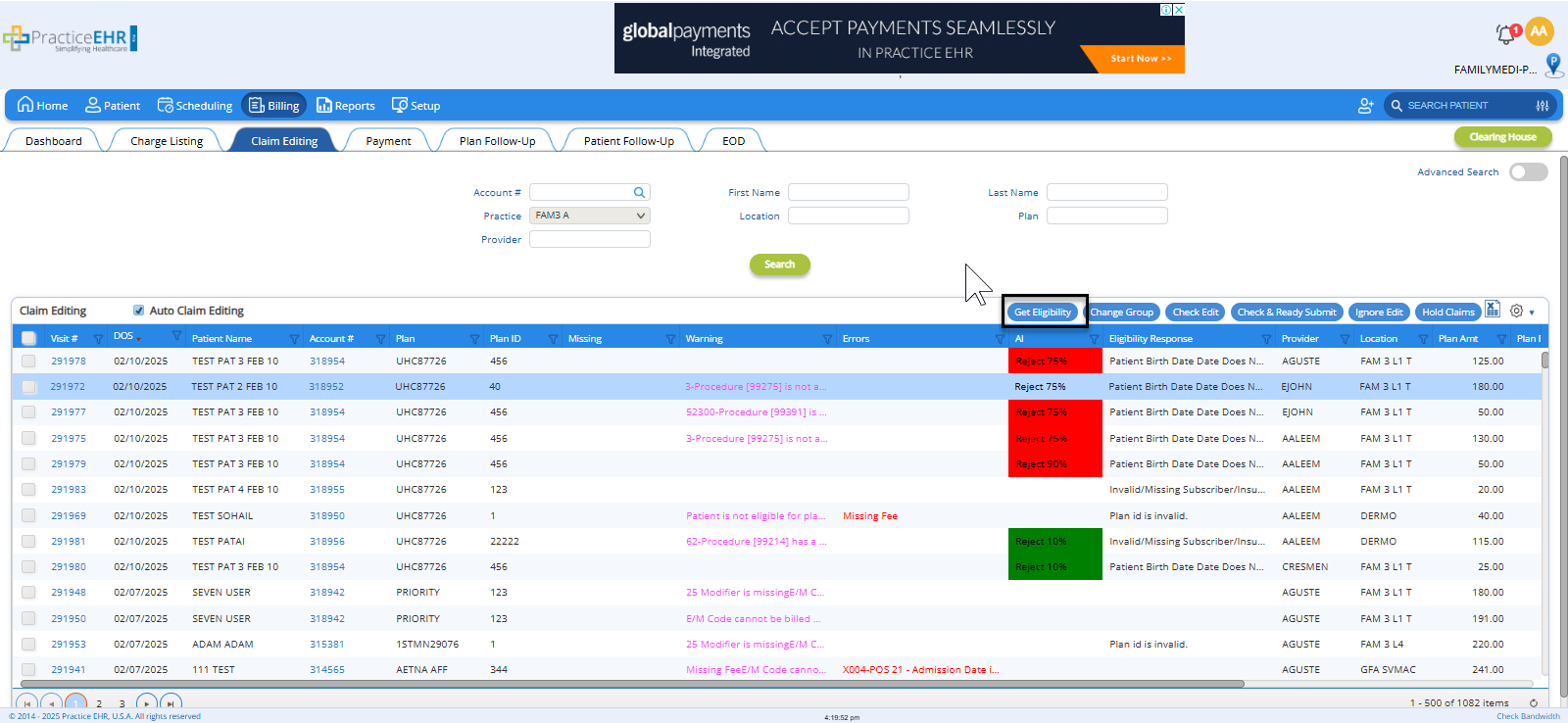
- New "Get Eligibility" Button in Claim Editing Bucket
- A new "Get Eligibility" button has been added to the Claim Editing Bucket. This button allows billers to request the eligibility status for the patient associated with the claim, ensuring they have up-to-date information before making submission decisions.
- Eligibility Response Columns Added to Claim Editing Grid
- Following the eligibility check, a new Eligibility Response column has been added to the Claim Editing Grid. This column will display the eligibility status of the patient for the specific claim, providing the biller with real-time data on the patient’s coverage and benefits.
- The eligibility response will include key details such as:
- Eligibility Status (e.g., Active, Inactive, Pending)
- Benefit Details (coverage limits, co-pays, deductibles)
- Plan Information (payer details and plan specifics)
- Eligibility Errors or Issues (if any)
- Decision Support for Billers
- By using the eligibility data, billers can make better-informed decisions about whether to proceed with a claim submission. For example:
- If eligibility is Active and coverage is sufficient, the claim can proceed to submission with confidence.
- If eligibility is Inactive or coverage issues are detected, billers can adjust or follow up with the patient before submitting the claim.
- This feature reduces the chances of claim rejections related to eligibility or coverage issues, streamlining the billing process and improving submission success.
6. PASSWORD EXPIRE FEATURE
Overview
To enhance security and ensure compliance with best practices, we have introduced a new Password Expiry feature in Practice EHR. This feature allows practice to set a specific time period (in days) after which all users in the practice will be required to change their passwords. When the password expires, users will be automatically redirected to the Password Change Screen to reset their credentials. This added layer of security helps protect sensitive patient data and strengthens overall account management. This feature is enabled by request only. Clients are requested to reach out to support for activation.